Primary care stands as the frontline of healthcare, where physicians are tasked with a broad spectrum of diagnoses, often relying on traditional methods of observation and examination. While medical imaging has seen remarkable advancements, its integration into primary care has been limited. Existing tools like otoscopes and ophthalmoscopes only allow for surface-level examination, missing crucial subsurface details that could significantly enhance diagnostic accuracy. This gap highlights a pressing need for advanced diagnostic tools that are practical, efficient, and effective in primary care settings. Addressing this need, the handheld optical coherence tomography (OCT) scanner for primary care diagnostics emerges as a transformative technology, promising to bridge the diagnostic gap and elevate the standard of primary healthcare.
I. The Imperative for Advanced Diagnostics in Primary Care
Primary care physicians are the cornerstone of the healthcare system, serving as the initial point of contact for most patients. Their expertise lies in navigating a vast landscape of medical conditions, making initial diagnoses, and guiding patients towards appropriate care pathways. However, the reliance on conventional diagnostic methods, heavily dependent on subjective symptom interpretation and physical examinations, can sometimes lead to diagnostic uncertainties, particularly in the early stages of complex diseases. Misdiagnosis or delayed diagnosis can have significant implications for patient outcomes and healthcare costs.
The advent of medical imaging technologies has revolutionized disease detection and diagnosis in numerous medical specialties. Modalities like MRI, CT scans, and ultrasound have become indispensable for detailed internal visualization. Yet, their size, cost, and operational complexities often render them impractical for routine use in primary care offices. The diagnostic toolkit in primary care is often limited to basic instruments. Otoscopes and ophthalmoscopes, while valuable for visualizing the ear canal, tympanic membrane, anterior chamber, and retina, are inherently limited to surface observation. Critical subsurface pathologies that could provide early indicators of disease remain undetected by these surface-centric tools. This limitation underscores the urgent need for innovative diagnostic solutions tailored to the unique demands of primary care, where efficiency, portability, and ease of use are paramount. The Handheld Optical Coherence Tomography Scanner For Primary Care Diagnostics is engineered to meet these demands head-on.
Optical coherence tomography (OCT) presents a groundbreaking solution to overcome these diagnostic limitations. OCT is an advanced imaging technique that provides high-resolution, cross-sectional views of tissue microstructure in real-time. It operates by detecting backscattered near-infrared light, creating detailed images of tissue beneath the surface. The ability to miniaturize OCT technology into flexible endoscopes, catheters, microscopes, needle probes, and crucially, handheld scanners, expands its applicability across diverse clinical settings. OCT’s non-invasive nature, rapid imaging speed, and high resolution make it exceptionally well-suited for integration into the fast-paced environment of primary care. Furthermore, the proven success of OCT in specialized fields such as ophthalmology, dermatology, and dentistry, demonstrates its broad diagnostic potential for conditions frequently encountered in primary care. Despite its clear benefits, the application of OCT technology in primary care medicine has remained largely unexplored until now.
This article introduces a novel handheld OCT scanner and system designed specifically for primary care diagnostics. This innovative tool empowers physicians to visualize not only the tissue surface but also the subsurface microstructure with high-speed OCT imaging. This capability offers the potential for more precise, quantitative diagnoses, providing digital 2D and 3D datasets that can be invaluable for clinical decision-making and collaborative patient care. The efficacy of this system has been rigorously evaluated through in vivo imaging of both human and animal tissues, demonstrating its practical applicability and diagnostic potential in primary care settings.
II. Materials and Methods: Engineering a Point-of-Care OCT System
A. Compact and Portable OCT System Design
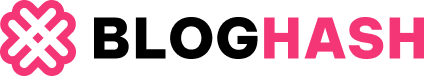
The development of our OCT system was guided by the specific requirements of a primary care environment. Space constraints and the need for rapid diagnostic assessments in primary care settings necessitate imaging systems that are both compact and capable of high-speed operation. Fig. 1 illustrates the spectral domain OCT (SD-OCT) system developed for this purpose, integrated into a portable medical cart (66 cm depth × 50 cm width × 94 cm height). This cart houses all essential components, including the light source, handheld OCT imaging scanner, computer, and monitor, ensuring mobility and ease of use within a clinic.
Fig. 1.
Schematic and photograph of the portable cart-based SD-OCT system, highlighting the handheld scanner. This system integrates optical components within a compact medical cart, ideal for primary care settings. The handheld scanner, connected via a 2-meter cable, offers flexibility for imaging various anatomical sites.
The SD-OCT system employs a fiber optic Michelson interferometer with a four-port configuration. A superluminescent diode light source, emitting at a central wavelength of 830 nm with a 70-nm bandwidth, provides approximately 4 μm axial resolution in tissue. Light is channeled through a 2 × 2 fiber coupler, splitting it into reference and sample arms. The sample arm incorporates the innovative handheld OCT scanner, connected via a 2-meter optical fiber and electrical wire, allowing for flexible maneuvering and patient access. This handheld OCT scanner features computer-controlled galvanometer mirrors and interchangeable lens mounts, designed to image diverse tissue types, including cornea, retina, tympanic membrane, oral mucosa, and skin, with a transverse resolution of ~15 μm. The reference arm includes switchable optical paths for retinal and non-retinal imaging, with dispersion compensation for retinal applications. Spectral interference signals are captured by a custom spectrometer, processed, and visualized in real-time, achieving an acquisition rate of 70,422 axial scans per second, or approximately 70 frames per second, with each frame comprising 1000 axial scans.
B. Handheld OCT Scanner: Design and Functionality
The handheld OCT scanner is meticulously engineered for clinical utility, housed in a lightweight and durable plastic enclosure (11.5 cm × 11.5 cm × 6.3 cm), as depicted in Fig. 2(a). Three interchangeable lens mounts are designed to ensure optimal tissue contact and imaging across different anatomical locations: retina, ear, and general tissues. Notably, the ear lens mount is adapted from standard otoscope ear tips, enabling the use of disposable specula for enhanced hygiene. All lens mounts are securely fitted within a 1-inch threaded lens tube, with focal lengths precisely calibrated for tissue contact imaging, as shown in Fig. 2(b). An integrated miniature CCD color video camera (1.6 cm diameter × 2.1 cm length, 0.27 megapixel) allows for real-time video imaging of the tissue surface during OCT scanning. This video guidance is critical for accurately positioning the OCT beam over specific areas of interest, facilitating precise correlation between surface features and subsurface OCT images.
Fig. 2.
Detailed views of the handheld OCT scanner and its components. (a) Interchangeable lens mounts, designed for various clinical applications, attach easily to the handheld scanner. (b) Demonstrates the handheld OCT scanner in use, showing its ergonomic design for physician operation during tissue imaging. (c) Illustrates the optical pathways within the lens mount, integrating OCT and LED illumination for simultaneous video and OCT imaging.
For video illumination, two red LEDs are strategically placed behind the focusing lens, preventing back-reflection and ensuring uniform lighting of the imaging site, as detailed in Fig. 2(c). LED operation is software-controlled, allowing users to adjust brightness via the imaging software. Physician operation is streamlined with integrated button controls on the scanner handle, enabling image capture and system control without additional assistance. This user-centric design of the handheld OCT scanner allows primary care physicians to efficiently target and image specific tissue regions in real-time, enhancing diagnostic workflow.
C. Enhancing Imaging Speed through Calibration and Software Optimization
Spectral domain OCT (SD-OCT) relies on wavelength-resolved spectral detection to determine tissue depth reflectivity. Maintaining a linear relationship between wave number and pixel position is crucial for accurate depth profiling; deviations can lead to point-spread function broadening and image distortion. Precise spectral calibration is therefore essential.
Traditional software-based spectral calibration methods, while convenient, can be computationally intensive, limiting imaging speed. To overcome this, we implemented a novel linear calibration method utilizing a translating-slit-based wavelength filter. This method acquires wavelength-pixel position data efficiently, measured automatically with a camera and optical spectrum analyzer. As a one-time calibration procedure, it eliminates the computational overhead during routine OCT imaging, significantly boosting speed. Furthermore, our imaging software, developed in Visual C++ with a multithreading architecture, maximizes parallel data processing and system control, ensuring efficient data communication and rapid image reconstruction. This combination of advanced calibration and software optimization significantly enhances the imaging speed of the handheld OCT scanner system, making it practical for real-time clinical applications.
III. Results: In Vivo Tissue Imaging with Handheld OCT
Under ethical approvals from the Institutional Review Board and the Institutional Animal Care and Use Committee, the handheld OCT scanner was evaluated through real-time 2D and 3D imaging of rat eyes and normal human tissues. Fig. 3 presents representative images demonstrating the system’s capabilities. Fig. 3(a) showcases reconstructed 3D images of a rat eye’s anterior chamber, displaying both top and angled views. 3D volumes (10 mm × 10 mm × 1.5 mm) were compiled from sequential 2D B-scans acquired and displayed in real-time, each B-scan consisting of 1000 A-scans with 2048 axial points. These images clearly delineate corneal and iris structures, even resolving fine details like eyelashes. 2D OCT images extracted from the 3D dataset further revealed detailed structural information at varying depths. Fig. 3(b)–(i) presents a series of 2D OCT images alongside corresponding video images of diverse in vivo human tissues, illustrating the system’s ability to capture intricate tissue morphology across different anatomical sites.
Fig. 3.
In vivo imaging results obtained with the handheld OCT scanner. (a) 3D OCT reconstructions of a rat eye anterior chamber, shown in angled and top views, reveal detailed ocular structures. (b-i) Paired OCT and video images of human tissues: (b) fingernail and fold, (c) uvula, (d) gumline mucosa, (e) arm skin, (f) cornea, (g) tympanic membrane, (h) retinal fovea, and (i) optic nerve head, demonstrating versatile diagnostic capabilities.
Specialized lens mounts facilitated imaging of different tissue types. The oral cavity lens mount included a protective cover glass and a focal distance of 2.5 cm, suitable for imaging as far back as the uvula. The ear imaging mount, equipped with a 2-mm aperture ear piece Fig. 2(a)], defined the lateral OCT image size, as shown in Fig. 3(g). For ophthalmic imaging, a soft eyecup on the lens mount ensured patient comfort, optimized focal length, and allowed for flexible angular adjustments for both anterior and posterior eye chamber imaging. While the current handheld scanner configuration does not provide simultaneous video imaging for ear and posterior eye chamber views due to fixed camera optics, video integration across all sites is achievable with camera modifications. The current video camera offers a 10° field of view, translating to a 2-cm video image at the OCT focal plane, with the video image center aligned with the OCT scan path Fig. 3(b)–(f)]. This co-registration of video and OCT images in space and time allows physicians to directly correlate surface visual findings with subsurface OCT data in real-time, enhancing diagnostic precision. The integrated design and user-friendly interface of the handheld OCT scanner streamline the entire imaging process, making it highly efficient for primary care settings.
IV. Conclusion: The Future of Point-of-Care Diagnostics with Handheld OCT
This study successfully demonstrates the potential of a new handheld OCT scanner and system as a practical point-of-care diagnostic tool for primary care. Designed to address the constraints of space and time in primary care settings, our system delivers rapid 2D and high-resolution 3D imaging, minimizing motion artifacts. While current imaging speeds are suitable for 2D and limited 3D applications, ongoing development focuses on enhancing speed for full volumetric in vivo imaging through advanced signal processing algorithms utilizing graphical processing units. Future iterations will prioritize ergonomic refinement and further miniaturization of the OCT unit to broaden its clinical utility.
The integration of advanced imaging technology like the handheld OCT scanner into primary care holds immense promise for improving diagnostic accuracy, enabling quantifiable data collection, and facilitating informed patient referrals. By enhancing the diagnostic capabilities of standard primary care instruments, particularly otoscopes and ophthalmoscopes, this technology can empower physicians to make more confident diagnoses, improve healthcare quality, and potentially reduce healthcare costs through earlier and more accurate disease detection. The handheld optical coherence tomography scanner for primary care diagnostics represents a significant step forward in transforming primary healthcare through innovative point-of-care technology.
Acknowledgments
This work was supported in part by research grants from the National Institutes of Health (NIBIB, R01 EB005221 and NCI, R21/R33 CA115536, S.A.B.), Blue Highway, LLC, Syracuse, NY, and Welch Allyn, Inc., Skaneateles Falls, NY.
The authors would like to thank C. Nguyen for her technical assistance, and Dr. M. Novak and Dr. S. Sayegh for their helpful medical discussions.
Contributor Information
Woonggyu Jung, Email: [email protected], Beckman Institute for Advanced Science and Technology, Urbana, IL 61801 USA.
Jeehyun Kim, Email: [email protected], School of Electronics Engineering, Kyungpook National University, Daegu 702-701, Korea.
Mansik Jeon, Email: [email protected], School of Electronics Engineering, Kyungpook National University, Daegu 702-701, Korea.
Eric J. Chaney, Email: [email protected], Beckman Institute for Advanced Science and Technology, Urbana, IL 61801 USA
Charles N. Stewart, Email: [email protected], Blue Highway, LLC, Syracuse, NY 13244-4100 USA, and also with Welch Allyn, Inc., Skaneateles Falls, NY 13152 USA
Stephen A. Boppart, Email: [email protected], Departments of Electrical and Computer Engineering, Bioengineering, and Internal Medicine, University of Illinois at Urbana-Champaign, Urbana, IL 61801 USA.