Electrophysiologists use specialized diagnostic tools to assess the electrical activity of the heart. Understanding what this diagnostic tool is called, how it works, and its importance in diagnosing heart conditions is crucial for both patients and medical professionals. This article will delve into the intricacies of this vital equipment, providing a comprehensive overview for anyone seeking to learn more about cardiac electrophysiology.
Understanding Cardiac Electrophysiology and Its Diagnostic Tool
Cardiac electrophysiology focuses on the heart’s electrical system. This system controls the heart’s rhythm, ensuring it beats regularly and efficiently. When this system malfunctions, it can lead to various heart rhythm disorders or arrhythmias. To diagnose and treat these conditions, electrophysiologists employ a crucial diagnostic tool: the electrophysiology study (EPS) system. This sophisticated technology allows them to pinpoint the source of abnormal heart rhythms and develop effective treatment strategies.
The Electrophysiology Study (EPS) System: A Deep Dive
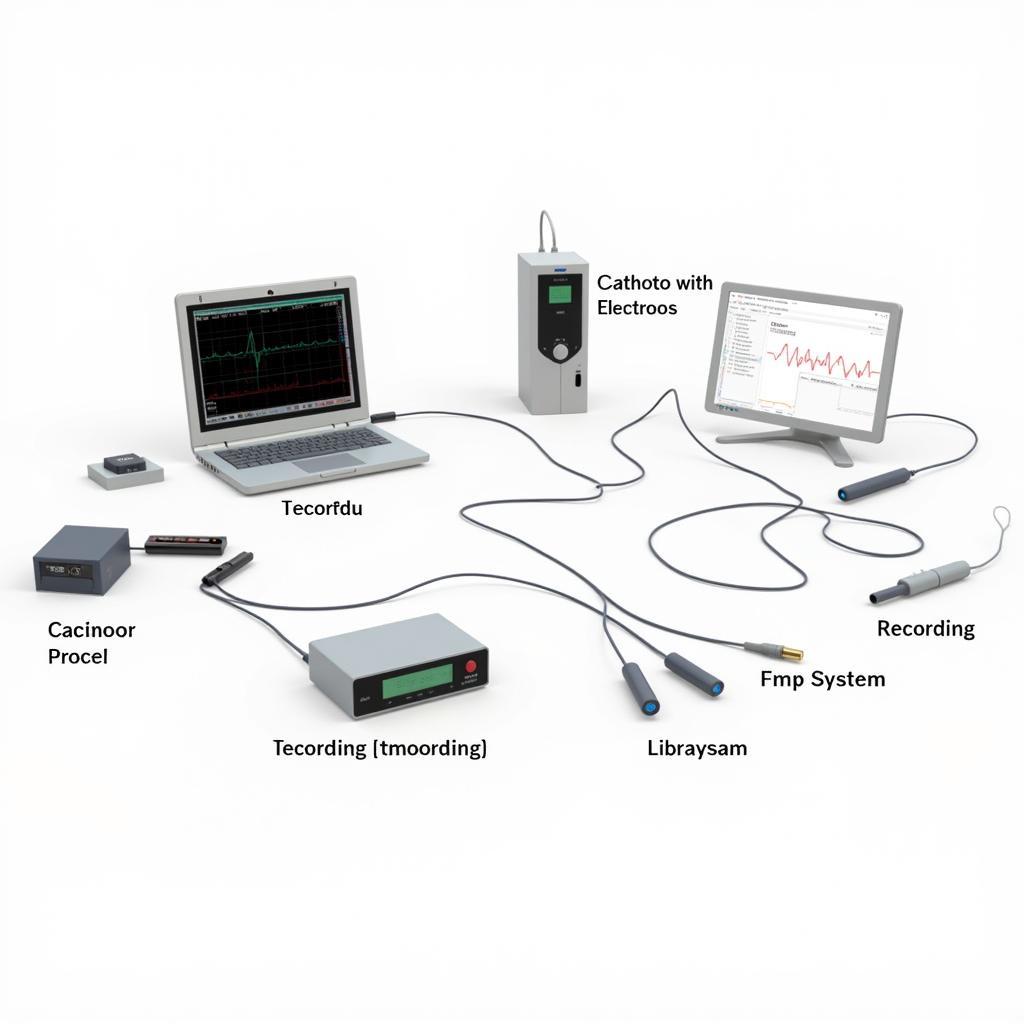
The EPS system isn’t a single device but rather a complex setup comprising several components working in concert. At its core are catheters, thin, flexible tubes inserted into a vein, typically in the groin or arm, and guided to the heart. These catheters are equipped with electrodes that can record and stimulate electrical activity within the heart chambers.
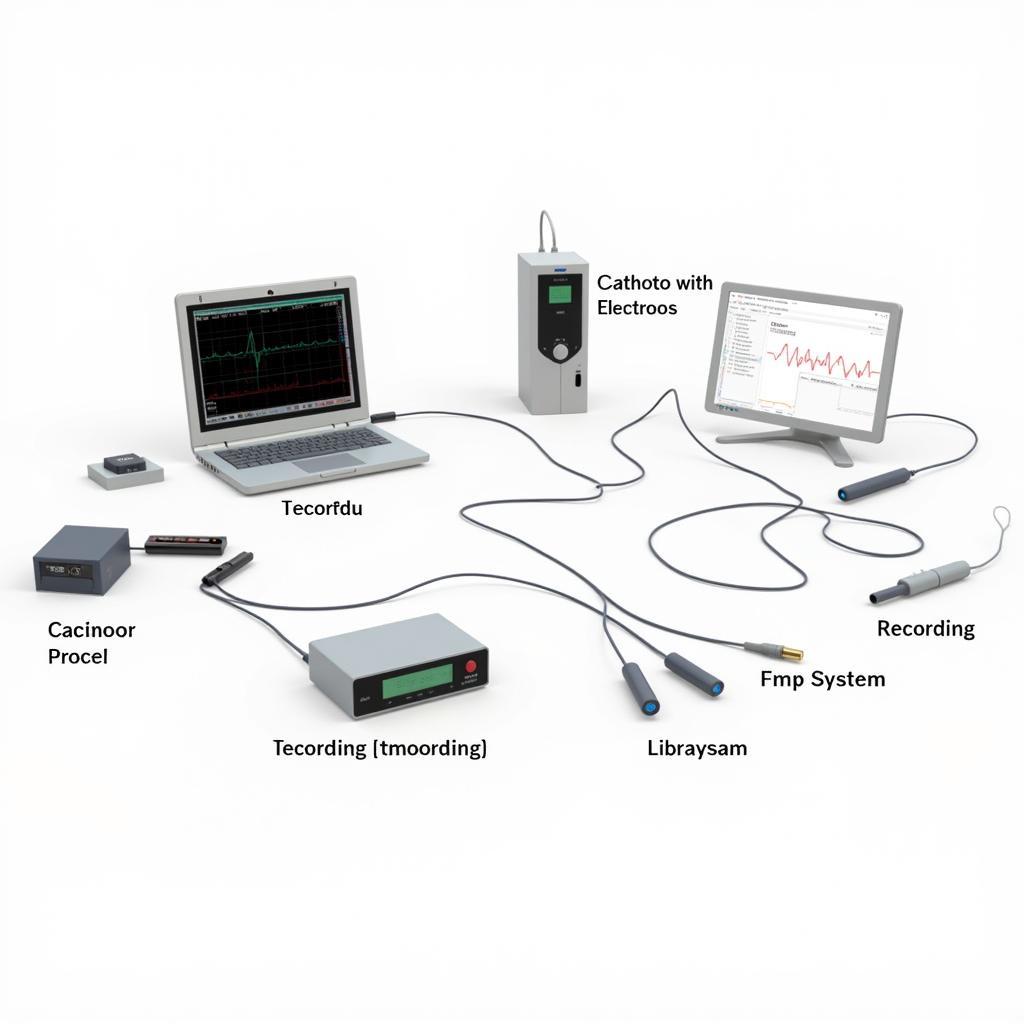 Electrophysiology Study System Components
Electrophysiology Study System Components
The electrical signals detected by the electrodes are transmitted to a recording system, which displays them on a monitor. This allows the electrophysiologist to visualize the heart’s electrical activity in real-time. Furthermore, the system can deliver precisely controlled electrical impulses through the catheters to stimulate the heart and induce arrhythmias. This controlled induction is vital for identifying the origin and mechanism of the abnormal rhythms.
Why is the EPS System Important?
The EPS system plays a crucial role in diagnosing and managing a wide array of heart rhythm disorders. It allows electrophysiologists to:
- Pinpoint the source of arrhythmias: By stimulating different areas of the heart, they can identify the precise location triggering the abnormal rhythm.
- Evaluate the effectiveness of medications: The EPS system helps determine how well antiarrhythmic drugs are working to control the heart rhythm.
- Guide treatment decisions: The information gathered during an EPS helps determine the most appropriate treatment strategy, which may include medication, catheter ablation, or implantation of a pacemaker or defibrillator.
Different Types of Catheters Used in EPS
Several types of catheters are used in EPS, each designed for specific purposes:
- Diagnostic Catheters: These catheters record the heart’s electrical activity and are used to map the electrical pathways within the heart.
- Ablation Catheters: These specialized catheters can deliver energy to destroy the tissue causing the arrhythmia. This procedure is known as catheter ablation.
- Mapping Catheters: These catheters are used to create a detailed 3D map of the heart’s electrical system, aiding in precise ablation procedures.
“The choice of catheter depends on the specific arrhythmia being investigated and the planned procedure,” says Dr. Emily Carter, a leading cardiac electrophysiologist at the University of California, San Francisco. “Each catheter provides unique capabilities, allowing us to tailor the procedure to the patient’s individual needs.”
Preparing for an EPS Study
If you’re scheduled for an EPS, here are some things you should know:
- Fasting: You’ll typically need to fast for several hours before the procedure.
- Medications: Your doctor will advise you on which medications to continue or discontinue before the study.
- Procedure Duration: An EPS can take several hours, depending on the complexity of the arrhythmia.
- Recovery: You’ll need to stay in the hospital for a short period after the procedure for monitoring.
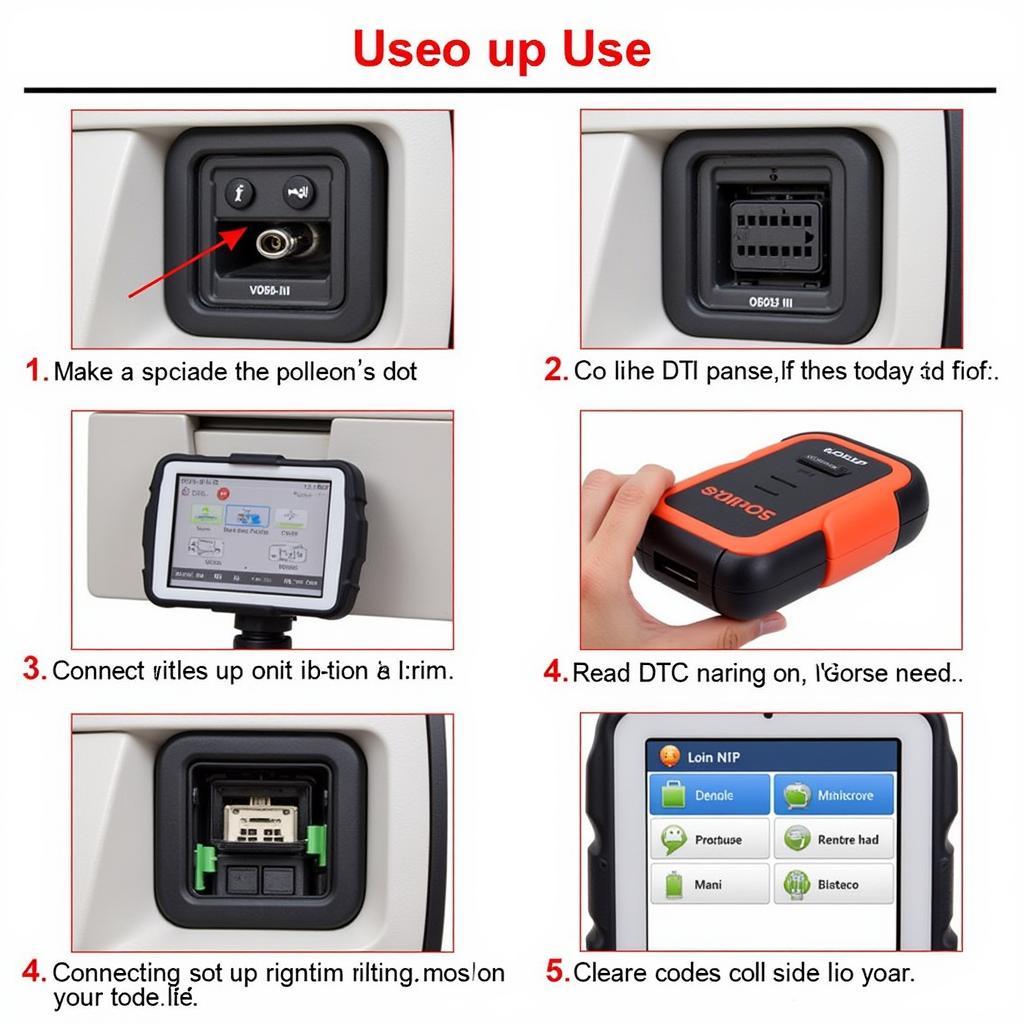
What to Expect During an EPS Procedure
During the procedure, you’ll be given a mild sedative to help you relax. The electrophysiologist will insert the catheters through a small incision in your groin or arm and guide them to your heart. You may feel some pressure or discomfort during the catheter insertion, but it’s generally not painful.
“Patients often ask about any pain associated with the procedure,” says Dr. Michael Davis, a renowned cardiac electrophysiologist at Johns Hopkins Hospital. “While some pressure is normal during catheter insertion, we take measures to ensure patient comfort throughout the procedure.”
Conclusion
The electrophysiology study (EPS) system, utilizing specialized catheters and recording equipment, is the essential diagnostic tool used by electrophysiologists to understand and treat heart rhythm disorders. By providing a detailed view of the heart’s electrical activity, this technology enables accurate diagnosis and effective treatment strategies, ultimately improving patient outcomes. If you’re experiencing heart rhythm problems, connect with a qualified electrophysiologist to discuss whether an EPS might be beneficial for you. We’re here to help. Contact CARW Workshop at +1 (641) 206-8880 or visit our office at 4 Villa Wy, Shoshoni, Wyoming, United States.
FAQ
- Is an EPS painful? While some pressure may be felt during catheter insertion, the procedure itself is generally not painful.
- How long does an EPS take? The duration of an EPS varies but can take several hours.
- What are the risks of an EPS? While generally safe, EPS carries some risks, such as bleeding, infection, or damage to blood vessels.
- What happens after an EPS? You’ll need to stay in the hospital for monitoring for a short period after the procedure.
- What can an EPS diagnose? An EPS can diagnose various heart rhythm disorders, including atrial fibrillation, supraventricular tachycardia, and ventricular tachycardia.
- What is catheter ablation? Catheter ablation is a procedure performed during EPS to destroy the heart tissue causing the arrhythmia.
- How do I prepare for an EPS? You’ll typically need to fast for several hours and adjust your medications as directed by your doctor.