Optical Coherence Tomography (OCT) has become an indispensable tool in ophthalmology, celebrated for its ability to visualize microscopic tissue structures and diagnose eye diseases. However, its potential in primary care settings, the frontline of medical diagnosis, remains largely untapped. This article explores the development and evaluation of a novel Handheld Scanner Primary Care Imaging probe, designed to bring advanced OCT capabilities directly to primary care physicians for enhanced screening and early disease detection across various tissue sites, including the eye, ear, and skin. Our findings demonstrate the transformative potential of handheld scanner primary care imaging in improving diagnostic accuracy and patient care in primary healthcare.
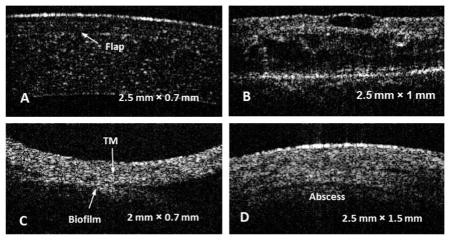
In vivo cross-sectional OCT images showcasing the diagnostic versatility of a handheld scanner in primary care settings. (A) Post-LASIK human cornea imaged with handheld scanner. (B) Advanced diabetic retinopathy visualized using handheld OCT. (C) Tympanic membrane biofilm detected by handheld scanner. (D) Skin abscess with fluid pockets, imaged with handheld OCT probe.
1. The Critical Need for Advanced Imaging in Primary Care
Primary care physicians are the cornerstone of healthcare, tasked with early disease detection and preventative screening for a broad patient population. They manage a high volume of patient visits annually, acting as the first point of contact for health concerns. Despite their crucial role, primary care physicians still rely heavily on traditional tools like otoscopes and ophthalmoscopes, which primarily offer surface-level tissue examination. These instruments, while fundamental, are limited in their ability to detect subtle, subsurface changes indicative of early-stage diseases.
The demand for primary care is growing, especially with an aging population, yet fewer physicians are choosing this specialty. This widening gap underscores the urgent need for more efficient and effective diagnostic tools in primary care. While medical imaging innovations have significantly advanced specialties like radiology and ophthalmology, primary care has not seen a similar technological leap. There is a clear opportunity to enhance primary care diagnostics with technologies that offer deeper tissue insights, quantitative data, and user-friendly designs.
Optical Coherence Tomography (OCT) emerges as a promising solution. This non-invasive optical imaging technique provides micron-scale resolution, real-time, 3D images of tissue microstructure. By measuring backscattered light intensity and time-of-flight, OCT creates detailed depth profiles up to millimeters beneath the tissue surface. Its non-invasive and non-ionizing nature has led to successful applications across diverse medical fields, including ophthalmology, cardiology, dermatology, and otolaryngology.
While OCT has revolutionized ophthalmology, its potential as a handheld scanner primary care imaging tool for broader primary care applications has remained largely unexplored. Early signs of many common pathologies present as subtle morphological changes at the micron level, such as retinal thickening, nerve fiber layer thinning, or biofilm formation. These changes are often undetectable with standard primary care instruments. Therefore, a handheld scanner primary care imaging device based on OCT technology could significantly enhance early disease screening and diagnosis in primary care settings.
To address this gap, we developed a portable OCT system integrated with a novel handheld scanner primary care imaging probe. Designed to resemble familiar instruments like otoscopes and ophthalmoscopes, this handheld scanner primary care imaging probe offers a user-friendly platform for physicians. Building upon our previous system, this improved design incorporates key advancements and has been clinically evaluated for its ability to identify early pathological indicators in common primary care examination sites, including the eye, ear, oral mucosa, and skin. This research aims to demonstrate the effectiveness of handheld scanner primary care imaging in transforming primary healthcare.
2. Advanced Design and Methodology of the Handheld OCT Scanner
2.1. Compact and Portable OCT System for Primary Care
The handheld scanner primary care imaging system is built around a fiber-based spectral domain OCT (SD-OCT) configuration, utilizing a superluminescent diode (SLD) light source and a commercial OCT spectrometer. The SLD emits light with a 70 nm bandwidth centered at 830 nm. The spectrometer encodes wavelengths onto a high-speed line scan camera, capable of capturing spectra at 70 kHz. B-mode images are constructed from 1000 A-lines. A fiber coupler splits the light into sample and reference paths, with a variable attenuator controlling reference path power. A flip mirror in the reference arm allows for dispersion compensation during retinal imaging, accommodating both anterior segment and retinal examinations.
Schematic of the portable OCT system integrated with a handheld scanner designed for primary care imaging. (A) System diagram showing key components: light source, spectrometer, and handheld probe. (B) Detailed anatomy of the handheld OCT scanner, highlighting the MEMS scanning mirror and ergonomic design.
The system, housed within a medical cart, connects to the handheld scanner primary care imaging probe via protected fiber and electrical connections. Figure 1A illustrates the OCT system schematic, along with a 3D model and photograph of the portable unit, showcasing its compact and mobile design suitable for primary care environments.
2.2. Ergonomic Handheld Probe for Enhanced User Experience
The handheld scanner primary care imaging probe serves as the physician’s interface with the patient. It houses a collimating lens to focus light from the delivery fiber onto a microelectromechanical systems (MEMS) scanning mirror, enabling beam scanning across the tissue. The beam exits through a port compatible with standard otoscope tips. Weighing 600g and ergonomically designed (10 cm × 11.25 cm × 5 cm enclosure with a 12 cm handle), the probe is comfortable and easy to maneuver. Figure 1B shows the anatomy of the handheld scanner primary care imaging probe.
A miniature CCD-based color video camera, operating at 25 Hz with 480 × 640 resolution, is integrated into the probe. This provides real-time video of the tissue surface, similar to a standard otoscope or ophthalmoscope, allowing physicians to visualize the OCT scanning beam location. A cold mirror separates the visible video path from the near-infrared OCT path. White-light LED illumination, delivered via fibers to the probe tip, enhances color video imaging of the tissue surface.
The probe features a metal tip for easy attachment and detachment of tissue-specific adaptors. Figure 2A and B display the handheld scanner primary care imaging probe with and without an ear speculum tip. Figure 2C shows various tip attachments designed for retinal, anterior segment, skin, oral mucosa, and ear imaging. The retinal attachment includes a focal length adjustment collar to accommodate individual patient eye variations.
Functionality and versatility of the handheld scanner for primary care imaging. (A, B) Handheld scanner with and without ear speculum tip, illustrating its adaptable design. (C) Interchangeable scanner attachments for diverse applications: retina, anterior segment/skin, oral mucosa, and ear. (D, E) Handheld scanner in use for eye and ear imaging, with integrated LCD screen. (F–H) Cross-pattern scanning demonstration, showing video image and orthogonal OCT cross-sections of a capillary tube.
2.3. Key Improvements for Enhanced Performance and Usability
Significant enhancements were made to the handheld scanner primary care imaging probe’s design. The most notable are the integrated LCD touchscreen and the MEMS scanner. The LCD touchscreen, located on the probe’s back (Figure 2D and E), displays both the CCD camera video and the OCT cross-sectional image in real-time, eliminating the need for physicians to look away from the patient during examination.
The MEMS scanner, replacing the previous galvanometer system, offers a compact form factor and enables faster scanning speeds. The four-quadrant MEMS scanner used allows for scanning across positive and negative tilt angles on both axes, resulting in a larger field-of-view and simplified alignment. With resonant frequencies of 323 Hz and 330 Hz in the x- and y-axes, and maximum tilt angles exceeding 15 degrees, the MEMS scanner provides versatile scanning capabilities. Its static actuation allows for variable scan speeds and arbitrary scan patterns, including raster, radial, and point scans.
The MEMS scanner improves system speed, limited only by the spectrometer’s line rate, and significantly reduces the probe’s footprint. Using a single mirror for dual-axis scanning enables truly telecentric light delivery, a feature not achievable with galvanometer pairs.
To further enhance usability for primary care physicians, an auditory focus indicator was implemented. This feature emits an intermittent tone when the tissue is near the OCT beam’s focus, with increasing repetition frequency as focus approaches. This auditory feedback is particularly helpful when imaging challenging sites like the tympanic membrane deep within the ear canal, facilitating rapid and accurate beam positioning.
Additional improvements include an ergonomic handle for comfortable use and a robust redesign that fully encases fibers and cables within the probe and tubing.
To provide real-time tissue structure feedback, an X-Y cross-pattern scanning mode was developed. Instead of just a single B-scan, this alternating pattern displays two orthogonal slices through the tissue volume, offering more comprehensive structural information without compromising real-time performance. Figure 2F–H demonstrates this cross-pattern scanning, visualizing transverse and longitudinal cross-sections of a capillary tube.
2.4. Clinical Evaluation on Human Subjects
Human subject protocols were approved by the Institutional Review Board at the University of Illinois at Urbana-Champaign. Six subjects were recruited: one control and five with various pathologies. Imaging was performed at The Eye Center in Champaign, IL, and the Beckman Institute for Advanced Science and Technology. The handheld scanner primary care imaging system and probe were used for all patient imaging.
3. Clinical Results and Discussion: Handheld OCT in Primary Care
3.1. Broad Tissue Site Accessibility for Primary Care Examinations
The handheld scanner primary care imaging probe demonstrated access to a wide range of tissue sites commonly examined in primary care. Figure 3 showcases in vivo OCT images of human tissues, including fingernail and fold, fingertip skin (sweat duct visible), oral mucosa, tooth and gum tissue, tympanic membrane, eye angle, cornea, retina, and optic nerve head. These sites are routinely assessed during general health exams, often requiring multiple specialized devices. The OCT images reveal subsurface details and structures at these sites that are undetectable with traditional surface imaging instruments used in primary care, highlighting the potential of handheld scanner primary care imaging to provide richer diagnostic information.
In vivo OCT images from a handheld scanner demonstrating broad tissue accessibility for primary care applications. (A) Fingernail plate and fold. (B) Fingertip skin showing sweat duct. (C) Oral mucosa at the gum line. (D) Tooth and adjacent gum tissue. (E) Tympanic membrane. (F) Eye angle revealing iris and sclera. (G) Cornea. (H) Retina fovea with retinal layers labeled. (I) Retina around the optic nerve head.
3.2. Pathological Observation and Screening Capabilities in Primary Care
Beyond normal tissue imaging, the handheld scanner primary care imaging probe effectively visualized various pathologies relevant to primary care. Figure 4 presents orthogonal cross-sectional OCT views of pathological conditions. Figure 4A and B show corneal images post-LASIK surgery, clearly visualizing the corneal flap. Figure 4C and D depict a tympanic membrane with biofilm from chronic otitis media, distinguishing between the smooth tympanic membrane and the less organized biofilm. Figure 4E and F show an abscess, revealing layer separation and fluid accumulation pockets due to infection.
Handheld OCT scanner images of common pathologies encountered in primary care. (A, B) Post-LASIK cornea, showing corneal flap. (C, D) Tympanic membrane with biofilm in chronic otitis media. (E, F) Skin abscess with fluid pockets and layer separation. Orthogonal (X-Z and Y-Z) planes are shown for each pathology.
To evaluate the handheld scanner primary care imaging probe for screening, retinal images were acquired from a control patient and three patients with varying stages of diabetic retinopathy. Figure 5 presents OCT retinal images, including a normal control and varying severities of diabetic retinopathy. Figure 5C and D show early-stage macular edema, characterized by retinal thickening. Figure 5E and F show more advanced macular edema with increased thickness and fluid accumulation. Figure 5G and H illustrate advanced macular edema with cysts and significant retinal thickening.
OCT images of diabetic retinopathy stages captured with a handheld scanner for primary care screening. (A, B) Normal retina. (C, D) Early-stage diabetic retinopathy with layer disturbance. (E, F) Diabetic retinopathy with macular edema and retinal swelling. (G, H) Advanced diabetic retinopathy with cysts and significant thickening.
While advanced diabetic retinopathy can be detected with a direct ophthalmoscope, early stages, like that in Figure 5C and D, are often difficult to identify using conventional tools. Early detection and intervention in diabetic retinopathy are crucial to prevent significant retinal damage, as demonstrated by the Early Treatment Diabetic Retinopathy Study (ETDRS). The handheld scanner primary care imaging probe’s ability to detect early-stage diabetic retinopathy highlights its potential for improving early diagnosis and timely referrals in primary care.
To further enhance the practicality of handheld scanner primary care imaging in busy primary care settings, automated image analysis methods are being developed. The goal is to provide physicians with simplified, quantitative outputs, such as a single number or binary classification (normal/pathological), to aid in screening and diagnosis, rather than requiring complex image interpretation.
OCT is already a valuable diagnostic tool in ophthalmology. Our results suggest its significant potential as a handheld scanner primary care imaging technology for broader screening applications. Subsurface imaging capabilities are critical for early disease detection, as many pathological processes begin beneath the tissue surface. By providing primary care physicians with advanced optical imaging, handheld scanner primary care imaging can enable earlier and more accurate diagnoses, quantitative assessments, longitudinal monitoring, and more informed referrals, ultimately improving patient outcomes and healthcare efficiency.
Cost is a key consideration for primary care adoption. Unlike specialists, primary care physicians require versatile equipment applicable to a wide range of conditions. Specialized, expensive desktop OCT systems are impractical for primary care. However, decreasing costs of key OCT components like light sources and spectrometers are making low-cost OCT systems increasingly feasible. A target price point of under US$10,000 for a handheld scanner primary care imaging unit is achievable in the near future, making it a potentially accessible and impactful technology for primary care practices.
4. Conclusion: Transforming Primary Care with Handheld OCT Imaging
We have successfully developed and evaluated a portable, handheld scanner primary care imaging device. Integrated with a user-friendly probe resembling standard primary care instruments, this technology aims to transform OCT from a specialist diagnostic tool to a primary care screening modality. Handheld scanner primary care imaging offers the potential for early disease detection, quantitative longitudinal assessments, and improved referral accuracy in primary care.
Our study demonstrated the handheld scanner primary care imaging probe’s ability to image a variety of in vivo human tissue sites relevant to primary care examinations. It effectively visualized pathologies such as post-LASIK cornea, infected middle ear with biofilm, and skin abscess. Crucially, handheld scanner primary care imaging successfully detected early-stage diabetic retinopathy, identifying retinal abnormalities before they would be visible with a standard ophthalmoscope. These findings underscore the significant potential of handheld scanner primary care imaging as a valuable screening technology, extending OCT’s benefits beyond specialized medical fields to the frontline of healthcare.
Supplementary Material
Author Bios
NIHMS479206-supplement-Author_Bios.docx
Acknowledgments
We thank Darold Spillman, Eric Chaney, and Jessica Taibl for their valuable contributions. This research was supported by grants from the U.S. National Institutes of Health (NIBIB R01 EB013723, and NIBIB R01 EB012479), and Sponsored Research Agreements from Welch Allyn, Inc. and Blue Highway, LLC. Further information is available at http://biophotonics.illinois.edu and http://2020eyecenter.com.
Footnotes
Author biographies Please see Supporting Information online.
References
[References]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Author Bios